Blind people use a cane to orient themselves in space and know where there are obstacles. Other animals naturally use sound, whiskers or other warning devices.
A blind dog also needs something to tell it when it is approaching an obstacle. Dennis Hacker, a veterinarian from California, told us how to manually make a “cane” for a blind dog.
Using an aluminum strip, which allows to give it the desired shape while providing a solid barrier for the dog, we make a ring that fits the harness, with a prudent angle so that it can turn its head and have mobility in it.
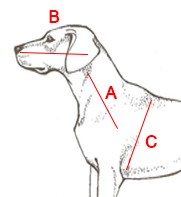
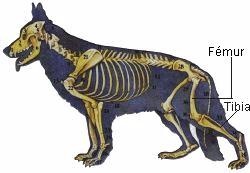
To manufacture it, we need to take 3 measures:
A – From the front leg to the neck.
B – From the neck to the tip of the nose.
C – The diameter of the chest just behind the front legs.
Necessary material:
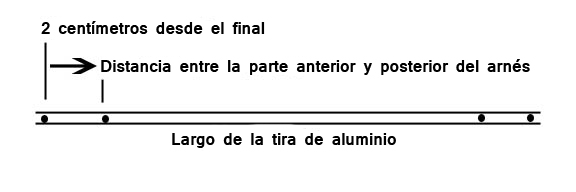
A – An aluminum strip of the correct size, these are the measures A + B multiplied by 3.
B – Leather harness, to fit on the chest. Remember that blind dogs tend to gain weight.
C – A riveting machine.
D – Rivets of 5 mm and 3-6 mm of reach.
E – Electric drill.
F – 5 mm helical drill bit.
G – Sandpaper.
The process for manufacturing is as follows:
Sand the edges of the aluminum so that they are round.
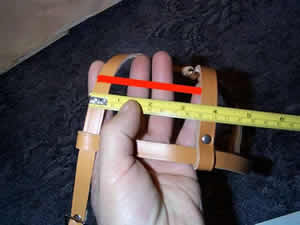
Attach the harness to the blind dog and adjust it to make it comfortable. It measures the distance between the centers of the vertical bands. This is where the ring-shaped aluminum bar is going to be put.
Drill four holes into the aluminum strip. A hole at each end and then another pair of holes at the distance between the two harness fasteners (as indicated in the photograph above left).
Pierce the harness at the bottom of the vertical strips of the neck where we measure. This is where the aluminum band is attached to warn the dog that it is about to hit itself.
Bend the distance to the ends of the aluminum bar with an angle of 45 degrees. Then, bend gently and in the opposite direction to give shape of circumference to the central area.
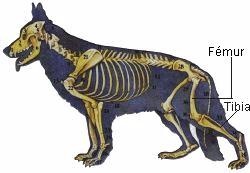
Rivet the aluminum ring to the harness on the vertical leather straps closest to the dog’s head.
Now, with the harness on the dog, level the hoop at eye and nose level. Mark the measurement and rivet the ring on the back of the harness.
We already have our cane ready for blind dogs!
The result is phascinating, a solution that will improve the lives of dogs with vision problems.
At first they feel confused and need to adapt, as soon as they understand the operation and see the improvement they quickly dodge the obstacles.
In case you are not one of those who have a lot of patience, the new harness for blind dogs is now available for sale.